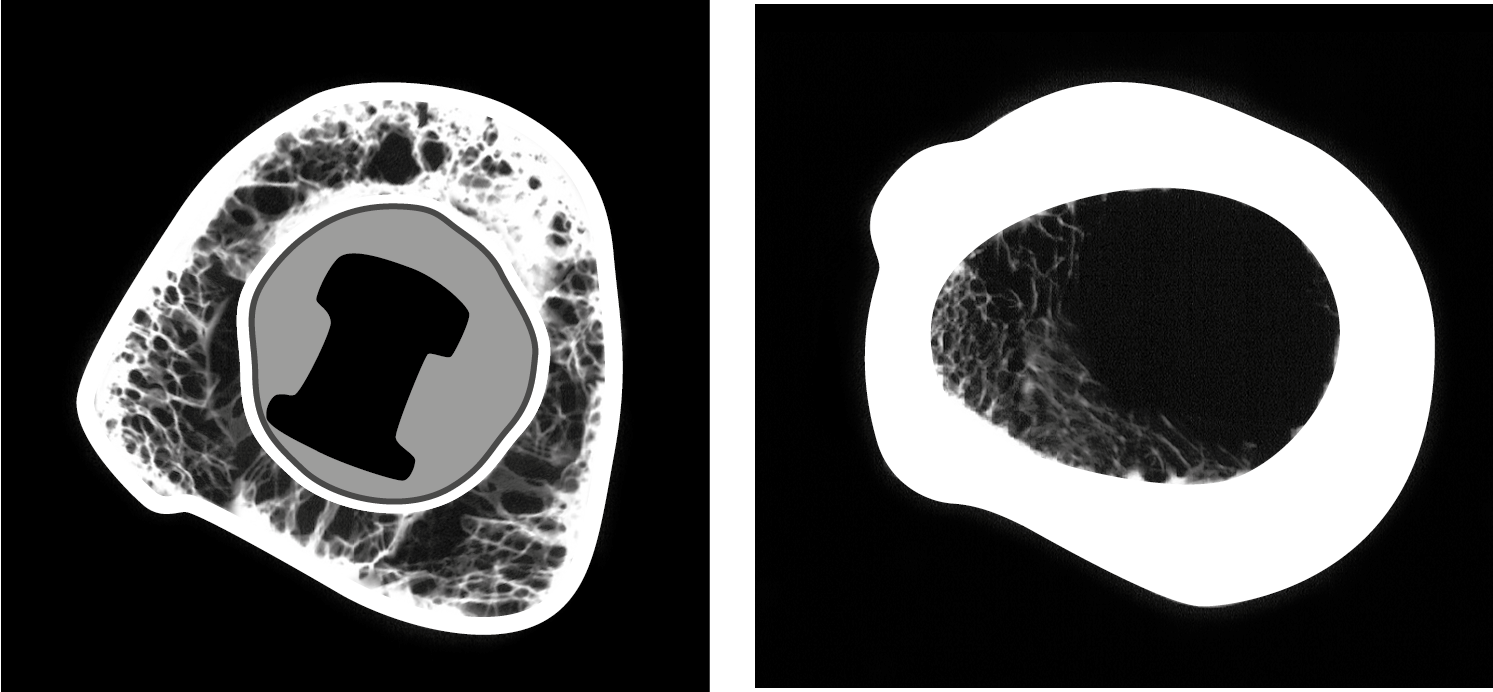
Fig. 1a: CT overview of a partially implanted mandible. The implants are integrated in the direction of the lingual cortical.
A Scientific Problem Analysis
Introduction
The term “periimplantitis” includes the suffix “-itis”. This leads our brains into the wrong direction. We tend to think that the origin of the disease is a bacterial attack and that we should use e.g. antibiotics to fight the disease and prevent progression. However, the clinical reality shows that antibiotic treatments are completely unable to stop the disease. This tells us that the origin of periimplantitis is not found in a bacterial attack, although bacteria might create an additional opportunistic infection which aggravates the disease and symptoms.
The occurrence of periimplantitis has been associated with a number of factors (depending on the author and their thought process), such as off-axis loadI, overloading of the crestal cortical in general, underloading of crestal bone, generalized diseases carried by the patient, plaque in combination with severe overloadingII, III or even with smoking.
The results of scientific investigation are not only inconsistent, but in fact very diverging. Surprisingly, a correlation between periimplantitis and (hormonal) osteoporosis has not been found.
Other factors have been discussed. Generally, the awareness of private dentists regarding the origin of periimplantitis is startlingly low, especially in countries with high incomes. Prevalence and clinical implications are generally underestimated. Typically, patients are not informed about this disease, even though it will affect nearly every patient to undergo treatment with conventional 2-stage implants.
The question of how to treat periimplantitis - or whether any successful treatment exists at all - has been investigated in depth. Answering this question remains difficult due to a number of factors: The term's definition is not globally agreed upon, it cannot be determined whether receding symptoms are caused by successful treatment or if the disease stopped «by itself», nor if the treatment attempt was successful in the long run.
We are also under the impression that any approach neglecting essential properties and bone function will never lead to a successful treatment concept.
Up to today the only safe way to avoid periimplantitis is the strict avoidance of rough-surfaced 2-stage implants.
As a result of their extensive analysis of literature, Heitz-Mayfield and MombelliIV reported that the disease re-appeared in 100% of the treated cases, with between 7% and 93% of the implants being affected again after a “successful” first treatmentVI. Esposito et al. showed in a thorough review that periimplantitis re-occurs in 100% of the cases after one year or later.
All literature on the treatment of periimplantitis available today refers to 2-stage implants with roughened surface, i.e. conventional 2-stage implants. While in earlier years laser treatment seemed to have prevailed, today (open) mechanical debridgement combined with (ineffective) antibiotic therapy seems to be the most frequently used “therapy“.
Few citations are available that relate to lateral basal implants. BOI® implants (belonging to the group of basal implants) appear to be free of this disease. Practitioners persistently using these implants world-wide claim they are not observing the occurrence of this disease at allVII. In the field of Strategic Implant®, this advantage is attributed to the thin and polished vertical implant shafts in combination with basal load transmission in the 2nd or 3rd cortical. The mechanical weight hits the bone far away from the crestal 1st cortical (i.e. the zone of bacterial attack). These implant designs do not show pockets around the mucosal penetration areas, nor has predictable vertical bone loss ever been ascribed to them.
Description and Interpretation of the Pathology
It is common in bone physiology to describe specific aspects of the bone's function in separate pictures. Viewing these pictures in entirety and assempling them into a "big picture of bone” allows a full understanding of bone funtionality VIII. We will use this exact technique of looking closely at specific developments or peculiarities of bone in order to detect different influences and possible causes of periimplantitis.
1st Question and Observations
Can we expect consistent and long lasting bone-to-implant-contact (BIC) around a (crestal) implant?
In traditional crestal implantology, the assumption prevails that dental implants should provide a large endosseous surface for better bone attachment. This would permit the transmission of stronge force though a large surface without overloading the bone. But in the clinical (histological) reality we find that even well integrated, long term implants show only 50% BIC, without signs of clinical deficiency (e.g. mobility). A higher BIC is found in the regions of cortical integration and under increased function.
2nd Question, Observations and Subsequent Analysis
Is “BIC” the same around the whole implant?
CT analysis of integrated implants show that the only implant surfaces showing high BIC are directed to a cortical. Surfaces directing in the longitudinal direction of the bone are hardly integrated at all.
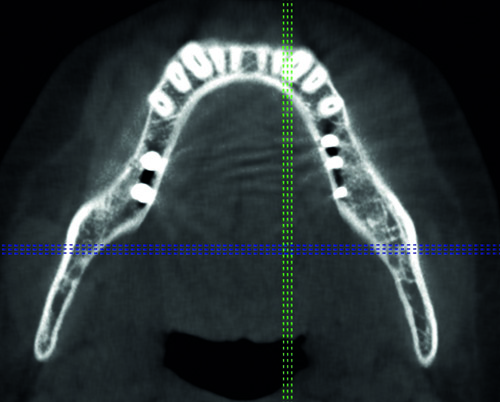
Fig. 1b: Well integrated single tooth implant in area 25. The implant is solely integrated in the direction of the corticals. Would specific surfaces (SLA, Ti-Unite, etc.) truly play a role in achieving and maintaining osseo-integration, we would not see a picture like this. Instead, the implant would be integrated evenly and all around with a high degree of mineralization.

These findings indicate that specific implant surfaces are of no importance for the long term integration of the implant. It is not possible to attract stable and mineralized bone to implant surfaces if the functional demand is not given.
3rd Question, Observations and Subsequent Analysis
Will we arrive at a logical interpretation of the origin of periimplantitis by applying “Wolff`s Law”?IX
Wolff`s Law includes (amongst others) the following aspects:
- optimization of a bone’s mechanical performance with respect to its weight
- alignment of trabeculae in the principal stress direction
- self-regulation of bone structure by cells reacting to a mechanical stimulus (i.e. through osteocytes)
- performance optimization through changes to the inner and outer morphology
- performance regulation through specific distribution of the mineralisation
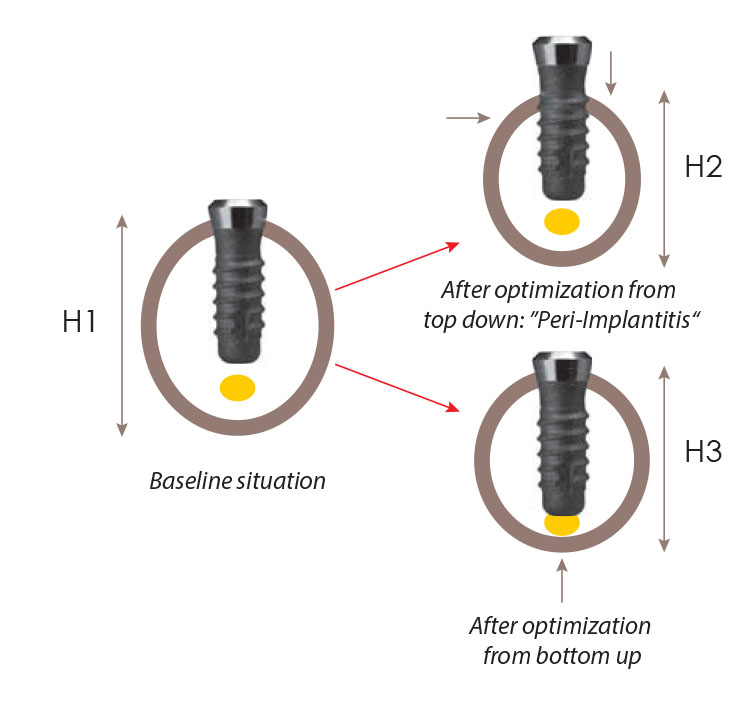
Bone loss around implants must be interpreted as such an optimization: It is clear that a lot of endosseous vascularisation (of the desmodontium) is lost after the extraction of teeth. Also, it is clear that too much bone is present after an extraction under functional aspects. In other words: any implant which is placed into severely atrophied bone may face periimplantitis. Non-appearace of periimplantitis is rather rare and considered the exception. This explains why up to 100% of the conventional dental implants are affected by this disease, and why therapy is not possible as long as bone is available in a functionally under-loaded situation in the vicinity of the implant. Note that any surgery on bone or injury of bone will always create local remodelling, which results in more bone loss (i.e. to an optimization according to Wolff`s Law).
Fig. 2c: Left (L): Ideally healed crestal implant with an even BIC of 50%. A higher BIC may develop in the crestal cortical areals (i.e. the implant‘s neck) and towards the lateral corticals (Fig. 2.e). Middle (M): Increase of BIC in the basal bone areas and simultaneous disintegration of bone. Full reduction (loss) of BIC (0%) at the crest, periimplantitis becomes visible. Right (R): A stable bone level is achieved as soon as the resorption has reached the border of the basal bone.
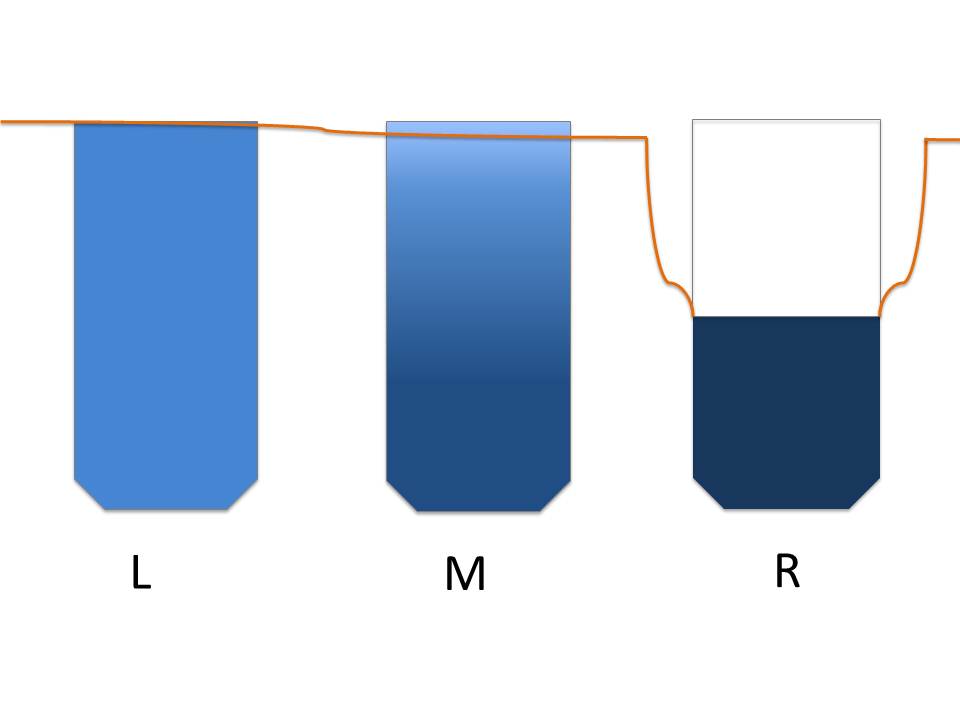
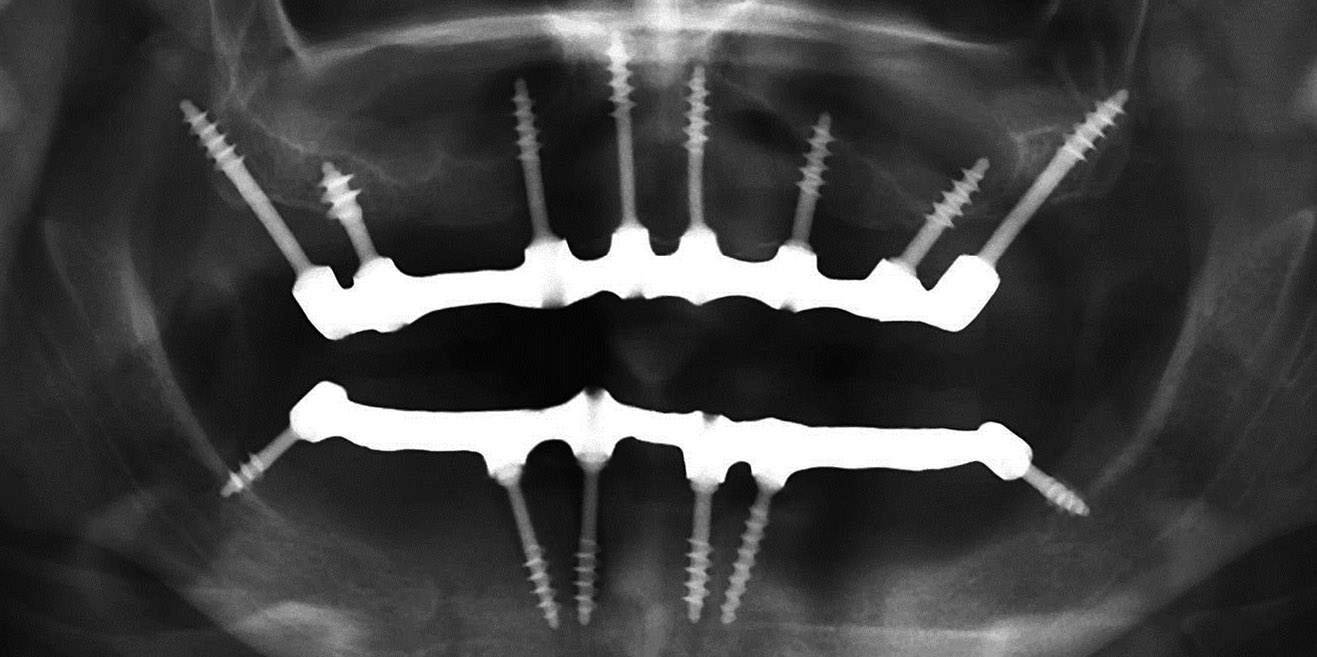
Fig. 2d: Although more than 50% of the vertical implant surface is exposed, the basal bone areas are holding the tips of the implants in the distal mandible. This situation resembles Fig. 2c (R).

4th Question, Observations and Subsequent Analysis
Is it true that a large endosseous implant surface (i.e. surface enlarging) is necessary for the success of an implant?
Both dental university research and teaching assume that implant surfaces must be as large as possible. The clinical observations on Strategic Implant® have shown however that minimal amounts of cortical bone can serve as a stable anchorage for implants even in immediate loading. Almost no bone is needed to load implants successfully as long as the bone is cortical. Osseo-fixation means in this context that the state of “osseo-integration” (direct contact between the implant body and living bone) is reached immediately when the implant is placed.
Fig. 2e: A short implant is integrated with a high degree of mineralisation, it is therefore able to transfer high loads into the bone. Appearance of periimplantitis in these designs is low because at this stage of atrophy, the occurrence of more atrophy is unlikely. We also learn from this observation that the rule of the crown length and endosseous length needing to be approximately 1:1 is clearly not valid even for crestal (2-stage) implants.
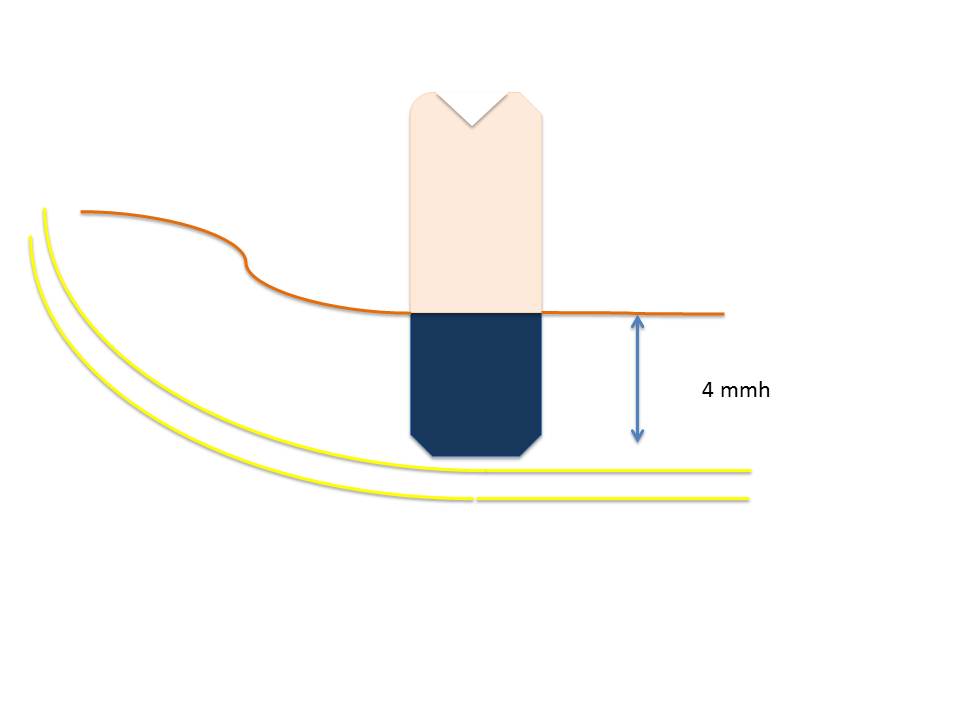
Fig. 2f: Two short BCS® implants are fixated in two corticals in the distal mandible. The total height of both corticals is approximately 3 mm. This means that not enough bone is present for the 5.5 mm thread of the implant at treatment onset. The situation has been stable for years, although the large bridge-span (according to university teaching today) also violates the rules of (traditional) implantology.
5th Question, Observations and Subsequent Analysis
Could "extra territorialisation", a development described by Prof. Karl Donath (Hamburg, 1935 - 2010), fit the appearance of periimplantitis and explain a part of it even better than today’s concepts?
During the time period when Prof. P. I. Branemark discovered and described “osseo-integration”, Prof. K. Donath invented the term ”extra territorialisation“. Both scientists described the same observations, but under different aspects and they ultimately postulated different reasons.
While P. I. Branemark assumed that bone actively recognizes surfaces, Donath pointed out the fact that any foreign surface will lead to a cortical encapsulation, a phenomenon he called “extra territorialisation”. He compared the cortical integration of an implant to the cortical encapsulation of a cyst. His explanation for the development included mainly mechanical reasons: cortical trajectories are formed to allow macro-trajectorial load transmission around the foreign body. According to this line of thought, a dental implant is a foreign body obstructing optimized osteon formation. Implants are blockages that integrate passively and block the optimization of macro-trajectories (i.e. pathways of secondary osteons).
Masticatory loads which are transmitted into the bone inside the implant may modulate bone formation once traction between the implant surface and bone has been achieved.
Fig. 2g: Typical pattern of trabeculation in a long bone. The bone is surrounded by a massive cortical. Black arrows indicate loads in both directions. The orientation and size of the spongeous trabeculae is determined by the mechanical demand (Wolff, 1982).
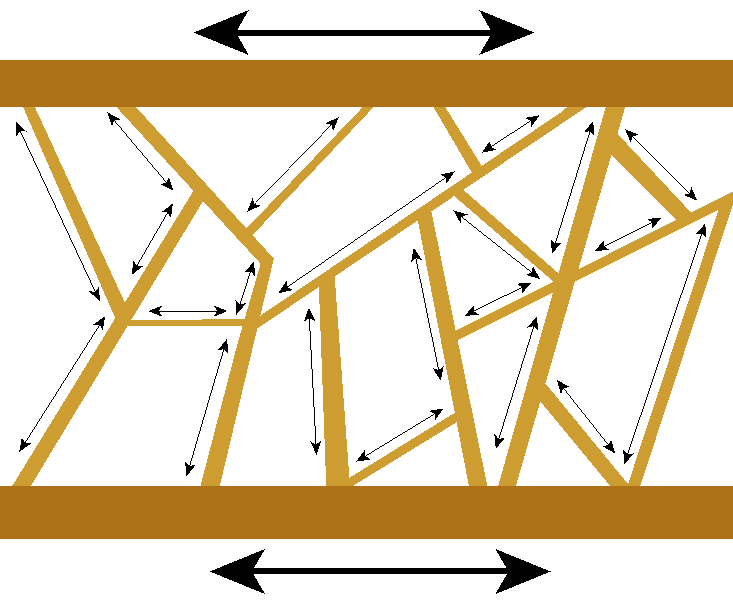
Fig. 2h: If a cyst develops in the bone (red ring =soft border, yellow = content of cyst), a completely new cortical develops (with or without (white) distance) to the soft cyst border.
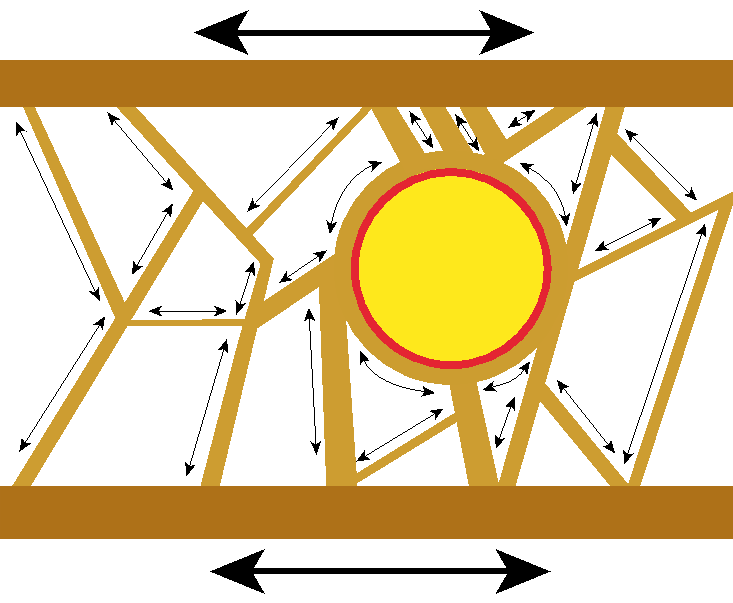
Fig. 2i: An osseo-integrated implant leads to the same type of changes inside the spongeous bone as around the cyst in Fig. 2h. Both developments have been defined as ”extra territorialisation“.
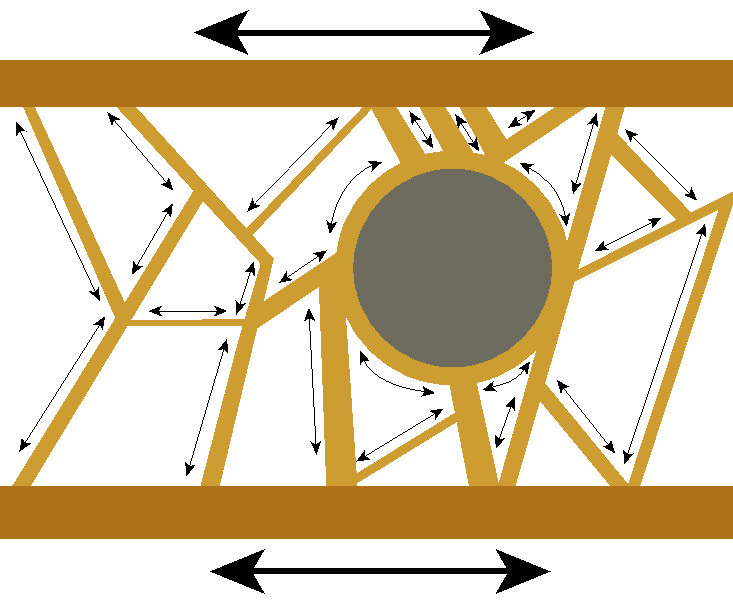
Fig. 2j: A cortical does not develop around granulations if they appear inside a bone. The metabolic activity of a granulation is much higher compared to a cyst. This prevents the formation of a mineralized cortical.
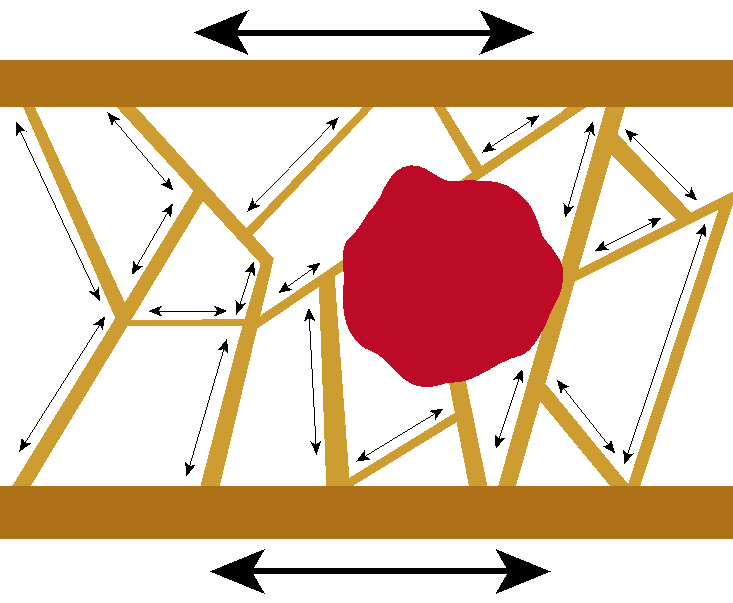
Fig. 2k: Left: Cemented shaft of a hip prosthesis 16 years post op. The bone around the cement has re-orientated through the process of self-trabeculation. Right: The non operated side of the same patient. These changes will occur around dental implants as well if the distance between bone and the implant provides space for such a redistribution of bone tissue.
6th Question, Observations and Subsequent Analysis
Does bone lose its natural elastic deformation (under regular functional load) if (overly) stiff crestal implants (by design and / or material) are inserted and osseo-integrate along the vertical implant axis?
Osseo-integrated 2-stage implants are ankylosed and the surrounding bone becomes increasingly stiff. One could call this status a “freeze” of the bone. Although extra territorialisation takes place and leads to higher mineralization, bone may still atrophy due to functional inactivity and due to the fact that reduced amounts of bone with high mineralization are required (Wolff's Law).
7th Question, Observations and Intepretation
Does splinting of crestal implants increase the crestal bone-loss?
RokniX et al (2005) and CochranXI et al (2009) showed that the vertical reduction of bone is increased with splinted implants (compared to single implants).
The cause of this additional bone loss may be found is a decreased functionality of the bone segment where conventional osseo-integrated dental implants are splinted.
8th Question, Relevant Observations and a Result
Are osseo-integrated implants bonded to the bone?
Everyone involved in creating histology with metallic implants in bone has observed that long term integrated implants easily detach from the bone. Unless macroretention is given, the metallic pieces simply fall out of the bone specimen. This is true for polished implants and for implants with any specific surface.
If implants are long term osseo-integrated into osteonal bone, the outer layer of each osteon is a fibrous tissue. This tissue layer does not provide any bond between implants and bone. Implants integrated into woven bone (callus) will also not bond sufficiently.
9th Question, Observations and Subsequent Analysis
How will the bone's structures behave under elastic deformations? Do implants influence the elasticity of the bone?
Histology shows:
- Osteonal bone consists of long tubes which spiral around and pervade each other. Bone lamellae of periosteal origin hold this cable bundle together around a long bone circumferential. Osteons are surrounded by a thin layer of soft tissue, i.e. they are not osseo-integrated against each other. One typical effect of tension on bone is an “osteonal pull-out”: single osteons are pulled out of a cluster of other osteons.
- Likewise, whole layers of osteons can start slipping against other such layers together. In this case we observe distinct “slip lines” inside the bone. Layers of bone or single osteons move against each other when bone deforms under function. If implants are integrated in this bone, they stop this deformation locally by blocking the slipping of single osteons against other osteons and / or the slipping of layers of osteons. Therefore, other layers (in the same region or others) must slip further or the whole bone segments becomes overly stiff. The distribution of mineralization is altered compared to bone not containing osseo-integrated implants.
10th Question, Observations and Subsequent Analysis
Does a rough implant surface influence the chances of re-integration of a mobile implant?
When we started working with lateral basal implants (disk-implants, BOIreg;) 20 years ago, all these implants were provided with a rough surface.
At that time, we regularly observed “periimplantitis” (crater-like bone loss) along the vertical axis of the implant. In some cases, this bone loss reached the base plate or even lower. In the case of pluri-disk-implants, only the basal base-plate resisted the tendency towards osteolysis.
We assumed that polished vertical implant parts were not as prone to this bone loss and after changing the design of the implant accordingly (polished vertical shafts with rough base plates), we found that no further periimplantitis occurred. These implants however still showed a slight tendency to reintegrate in the case of mechanical overload: mobilized base plates only rarely reintegrated, even if the load situation was corrected and no deep infection had occurred.
To understand this phenomenon, we have to remember that newly formed osteonal bone matrix is a soft tissue and if rough surfaces “rub” against soft tissues, the friction will alter or even destroy this tissue. This triggers the formation of a new osteon and the mineralisation will likely be reduced.
When we started to produce completely polished lateral basal implants, this phenomenon disappeared: as soon as the mechanical overload was corrected, the implants reintegrated and the surrounding bone reached a high degree of mineralisation within a few months (well visible on the x-ray).
From this experience we gather that
- polished vertical implant parts severely reduce the occurrence of a periimplantitis
- polished intra-osseous implant parts in general allow reintegration of implants that have been mobilized, usually due to mastication derived cyclic overload
- lateral mobility of the screwable basal implant is treated by correction of loads. Strong vertical mobility usually requires the exchange of the implant
11nd Question, Observations and Subsequent Analysis
Does the term “osseo-integration” include a situation where implants will change their spatial relationship relative to the surrounding bone in which they are integrated?
In question 3, we have already discussed the aspect of post-operative remodelling on the bone level at the crest of the implant. Fig. 2m illustrates the changes in morphology and the result on the bone-level.
Fig. 2l: If bone optimizes its structure, the total bone mass will be reduced (Wolff`s Law). Depending on where exactly the bone is modeled, we will sometimes find signs of a periimplantitis (upper right graph) or implant success (lower right graph) while the bone is reduced in another area. Note that endosseous resorption might also take place with no visible outer changes at all. This is fortunate: Imagine if the bone would always disappear from the crest, we would see much more periimplantitis than today in the clinical reality.
Summary
When viewing the above considerations, it becomes clear why the undisputed reasons for periiimplantitis have not been identified until this day. Clinical observations indicate that bacteria colonize the exposed rough implant surfaces, but this is no proof for the assumption that bacteria are the initial cause for the disease. In the field of basal implantology, we assume instead that the appearance of bacteria is opportunistic and takes place right after the bone has been demineralized enough to begin to shrink (i.e. optimize). The development of a clinically visible infection depends on the implant`s surface.
It is necessary to distinguish between the infection in the bone (mainly caused by invisible pre-operative intra-bony infections, see Fig. 2j) leading to early loss of implants with rough surfaces and periimplantitis.
From our experiences whith basal implantology during the past 25 years, we can conclude today that implants which feature:
- load transmission far away from the (unreliable) crestal bone
- thin mucosal penetration diameters of the implant
- polished (thin) penetration areas
allow the avoidance of periimplantitis in all cases, regardless of the cooperation of the patient and their willingness to take care of oral hygiene.
Acknowledgement:
The International Implant Foundation (Munich / Germany) thanks Prof. Dr. Stefan Ihde (prof(at)ihde.com) for providing this analysis.
[I] Uribe R, Peñarrocha M, Sanchis JM, García O Medicina Oral : Organo Official de la Sociedad Espanola de Medicina Oral y de la Academia Iberoamericana de Patologia y Medicina Bucal [2004, 9(2):160-2, 159-60.
[II] van Steenberghe D1, Naert I, Jacobs R, Quirynen M. Influence of inflammatory reactions vs. occlusal loading on peri-implant marginal bone level. Adv Dent Res. 1999 Jun;13:130-5.
[III] Heitz-Mayfield LJ1, Schmid B, Weigel C, Gerber S, Bosshardt DD, Jönsson J, Lang NP, Jönsson J. Does excessive occlusal load affect osseo-integration? An experimental study in the dog., J. Clin Oral Implants Res. 2004 Jun;15(3):259-68.
[IV] Heitz-Mayfield LJ, Mombelli A. The therapy of peri-implantitis: a systematic review. Int J Oral Maxillofac Implants. 2014;29 Suppl:325-45.
[VI] Esposito M1, Grusovin MG, Worthington HV Treatment of peri-implantitis: what interventions are effective? A Cochrane systematic review. Eur J Oral Implantol. 2012;5 Suppl:S21-41.
[VII] Ihde S., Principles of BOI. Textbook, Springer Heidelberg, 2005.
[VIII] Martin R.B., Burr D.B., Sharkey N.A.: Skelettal Tissue Mechanics, Springer, New York ;1998, ISBN 0-387-98474-7, www.springer-ny.com
[IX] Wolff J., Das Gesetz der Transformation der Knochen, Springer, Berlin, Germany, 1892 (in Germany)
[X] Rokni, S., Todescan, R., Watson, P., Pharoah, M., Adegbembo, A. O. & Deporter, D. 2005. An assessment of crown-to-root ratios with short sintered porous-surfaced implants supporting prostheses in partially edentulous patients. Int J Oral Maxillofac Implants, 20, 69-76
[XI] Cochran, D. L., Nummikoski, P. V., Schoolfield, J. D., Jones, A. A. & Oates, T. W. 2009. A prospective multicentre 5-year radiographic evaluation of crestal bone levels over time in 596 dental implants placed in 192 patients. J Periodontol, 80, 725-33




