Periimplantitis
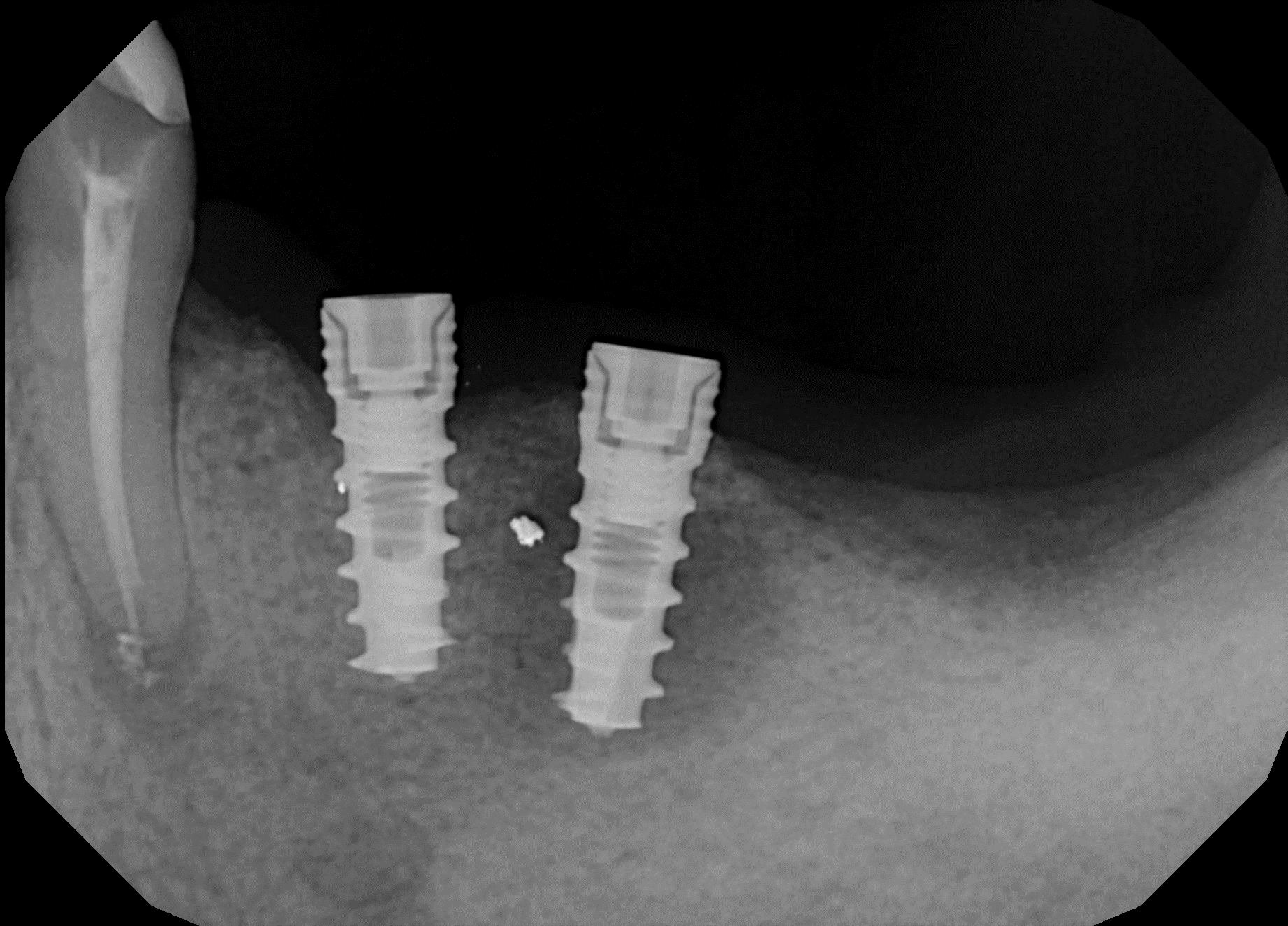
Periimplantitis occurs after the successful osseo-integration of the implant. This is especially unfortunate, since the disease starts to attack just as everything looks fine and the patient starts using the implant. Periiimplantitis starts at the oral cortical and leads to its increasing erosion. Periimplantitis is distinguished from the endosseous rest-ostitis, which typically stems from a reactivation of older, dormant root infections (Fig. 1).
Mild Cases
In mild cases, bone loss around the implant is 1-3 mm with some weak signs of inflammation of the mucosa, which may cause mild pain. These cases are treated symptomatically with local disinfectant and pain medication. It is known today that antibiotic therapy is not successful in stopping the progression of periimplantitis (regardless of the severity).
Medium Cases
In cases of medium severity, around 50% of the vertical bone along the implant is lost. The main problems are the recurrent emergence of pus and bleeding, the unsightly aesthetic appearance and foul smell.
Severe Cases
In serious cases of periimplantitis, nearly all bone matter gets resorbed, and deep soft tissue pockets result. Constant infection, discharge and heavy bleeding are the results. When pockets are surgically removed, the teeth's appearance strongly deteriorates and enormous amounts of food get stuck between the implants and bridges (Fig. 1, Fig. 2).
What Are The Causes of Periimplantitis and the Reasons for Its High Prevalence?
The oral cavity holds millions of bacteria which are typically washed away by drink, food and saliva. These bacteria settle on all hard surfaces inside the mouth and will multiply in favorable conditions. We know this from our own teeth.
The problem with almost all conventional 2-stage implants is that they are manufactured with a rough endosseous surface. This is done to achieve a strong grip between the implant and the bone, a strong osseo-integration.
We know today that bone will retract 1-3 mm along all such implants within the first months of usage. Rough implant surfaces will become exposed and quite likely colonized by bacteria.
The typical dental implant patient has lost their teeth due mainly to a persistent lack of sufficient oral hygiene (i.e. negligence). In other words: the «non-cleaners» within the population receive their implants earlier than others. However, conventional dental implants with rough surfaces and large diameters require an substantial amount of oral hygiene to stay infection-free.
In conclusion, these 2-stage implants with rough «endosseous» surface are quite unsuitable from the start for a large group of patients within the population. Additionally, most conventional 2-stage implants provide enormous amounts of endosseous implant surface, much more than necessary for load transmission purposes. Since a lot of bone-to-implant-contact requires functional stimuli, vertical bone loss along the implant is expected anyway.
Another general problem with conventional 2-stage implants is their utilization of the crestal cortical and underlying spongeous bone. These bone areas are already prone to resorption. This again leads to exposed implant surfaces that quickly hold a reservoir of bacteria and cause chronic infection and progressive bone loss. In this light, most 2-stage implants are in principle a faulty design and should be forbidden or their indications severely reduced.
Treatment of Periimplantitis
Even by now, there is no effective (final) treatment for this disease. All attempts at cleaning the infected areas remain ineffective due to oral bacteria multiplying hourly and perpetually, creating millions of new bacteria at every moment. Attempts at «polishing» the rough surfaces in the mouth do not work either, as such polishing is not possible close to the bone since remnants of the polisher remain on the implant and in the deep pocket, fostering new inflammation.
In some cases, periimplantitis stops on its own when the bone loss reaches resorption-resistant «basal» bone areas.
It is generally admitted today that reliable and successful treatments for periimplantitis are missing. Science still hopes to find such treatments:
Review of the treatment protocols for peri-implantitis.
The only way to avoid this disease with 100% certainty is to remove the 2-stage implant.
Level of Awareness of Treatment Providers Regarding Periimplantitis
The Swiss Monthly Journal for Dentistry published a survey among active swiss dentists regarding their knowledge on the topic of periiimplantitis.
It is not surprising that almost all answers by the polled swiss dentists were wrong by today's standard. Here is an overview:
| Suggested reasons for periimplantitis (%) |
| Periodontitis | 79.7 | 0.194 | 72.0 |
| Smoking | 76.9 | 0.365 | 71.4 |
| Bad Compliance | 53.2 | 0.247 | 60.9 |
| Parafunction | 20.3 | 0.618 | 23.1 |
| Smooth Implant Surface | 24.4 | 0.126 | 16.2 |
| Rough Implant Surface | 31.6 | 0.914 | 32.3 |
| Short Implants | 17.7 | 0.012 | 7.1 |
| Reduced Diameter | 16.5 | 0.008 | 6.0 |
| After Sinuslift | 10.1 | 0.999 | 10.1 |
| After Augmentation | 21.5 | 0.799 | 20.1 |
| After Immediate Loading | 31.6 | 0.671 | 29.0 |
| Knowledge of CIST (%) | 61.5 | 0.001 | 39.8 |
Only 31.6% of the survey's participants were able to identify «rough implant surfaces» as the reason of periimplantitis. The other two main reasons,- multipart implants and a large mucosal penetration diameter - were not mentioned at all by active swiss dentists.
Résumé: The awareness of swiss dentists regarding this important topic was extremely poor at the time of questioning. The survey reveals that no factual data is taught in either university education nor post-graduate training. We assume that this is owed to the strong influence of major implant manufacturers on the teaching of universities.
We are convinced that polls in most western countries would achieve equally shocking results. Not not only is knowledge apparently lacking, but also common sense (which would lead to correct results on such a simple question).
Conclusion
The very questionable design of most 2-stage implants (2-piece-design, large diameters, rough endosseous surfaces) is the main cause of this wide spread problem that severely affects the patient's quality of life. The design of the conventional 2-stage implants is unsuitable for use in a constantly infected oral environment. This feature of the implants is predominantly reponsible for the fact that no effective treatment exists for periimplantitis.
Our reccomendation is to avoid such implant designs. These days, after the development of «basal implants» (Strategic Implant®), safe alternative treatment devices and techniques are available. They prevent this severe clinical problem without any similarly serious side effects.